An Illinois Public Radio story caught my eye on Twitter this week. It dealt with a major player in Chicago charter schools and their disciplinary policies. Limitations on bathroom usage meant many young women were bleeding through the mandatory khaki pants during their periods, a less than ideal situation for all involved:
An Illinois Public Radio story caught my eye on Twitter this week. It dealt with a major player in Chicago charter schools and their disciplinary policies. Limitations on bathroom usage meant many young women were bleeding through the mandatory khaki pants during their periods, a less than ideal situation for all involved:
“We have (bathroom) escorts, and they rarely come so we end up walking out (of class) and that gets us in trouble,” she texted. “But who wants to walk around knowing there’s blood on them? It can still stain the seats. They just need to be more understanding.”
They go on to defend the policy, noting that girls who bleed through their pants can tie a sweater around their waist to cover up the damage. Of course, since this is not a usually acceptable part of the dress code, they then announce the names of the girls who are allowed to wear this aberration.
Yeah, please announce to the world the name of the menstruating students. Nothing about that will make them feel self-conscious or awkward.
I haven’t worried about bleeding through for a while now, but I do worry about bathroom access in schools. As a pediatric nephrologist, I take care of a lot of children who would benefit from easier access to the restroom.
- First up are those children with frequent urinary tract infections (UTIs). One of our defenses against UTI is completely emptying our bladders on a regular basis. This action flushes out any bacteria that have made their way into the interior space. In addition to that, holding urine can cause the bladder to lose efficient function. Children may not be able to empty completely, meaning bacteria are more likely to get a foothold in the bladder and cause trouble.
- Second, we must consider children with constipation. A large wad of poop can put pressure on the bladder, its outlet, and its nerves, preventing proper sensation and function. These children must be cleaned out with aggressive stool softening. How inconvenient if the bathroom escort is not available when the poop is ready to pop! Holding it in not only makes constipation worse but further worsens bladder function and makes UTI likely. Adequate fluid intake can also prevent constipation.
- Third, a lot of children get kidney stones. Some of these kids have biochemical problems that can be treated, but even those stone-formers could likely prevent such things if they drank enough water. For adults, we recommend enough water to produce 2 liters (66 oz) of urine daily. This means drinking 2-2.5 liters of fluid. At least part of this should be consumed during the school day, necessitating bathroom use. Kidney stones produce debilitating pain, and in the long-run can lead to permanent kidney damage.
Other considerations include keeping bathrooms clean and functional and safe.
I would like to declare that all people, even students, have the right to use the bathroom when necessary. Not only is holding pee and poop in harmful, but I cannot imagine being able to learn when I’m worried about losing control or bleeding through my clothing.
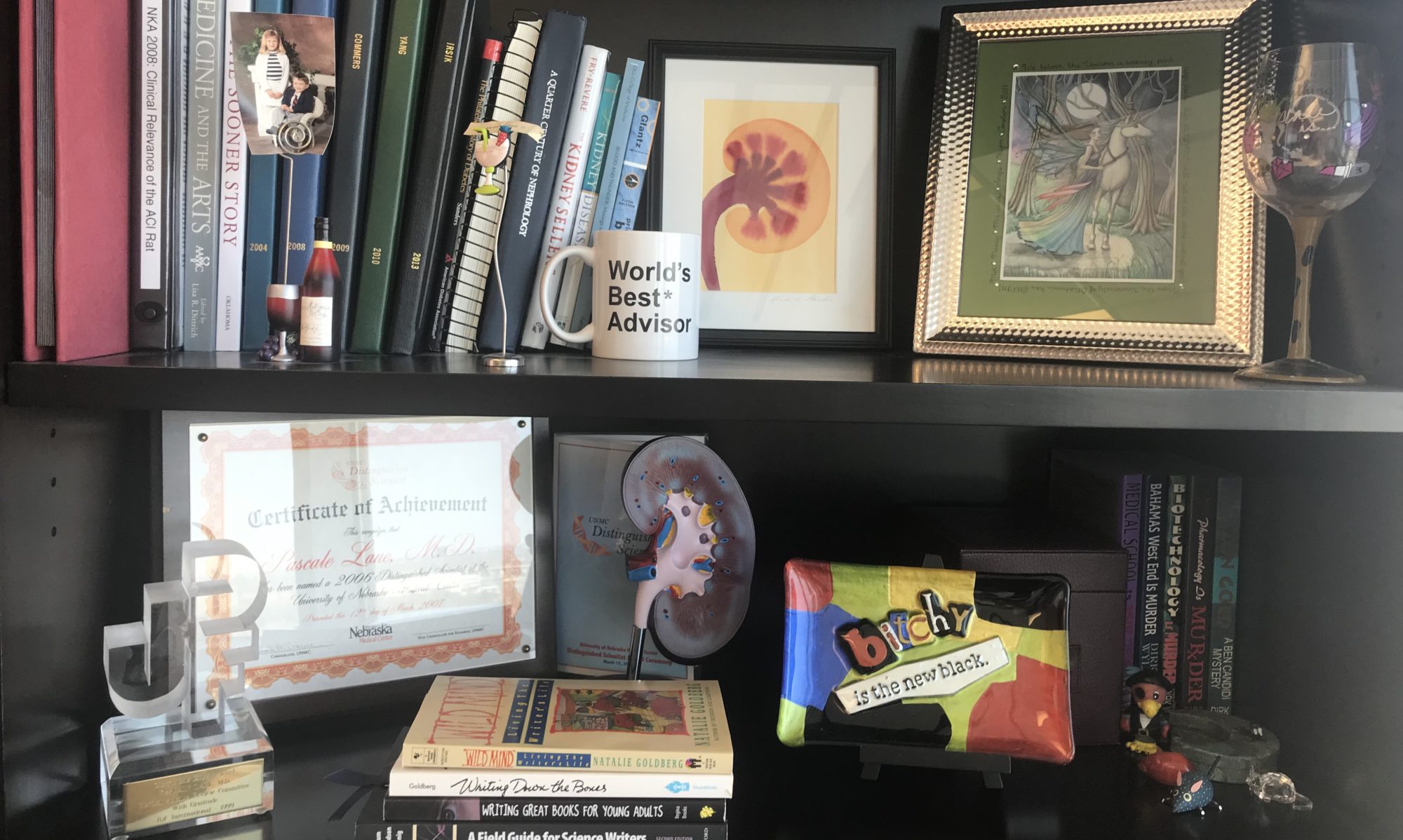
Join me in showing support for the right to hygienic elimination! You can buy a “Let Kids Pee” ceramic cup or stainless steel travel mug on Amazon (my design is featured above in this post). You will help support this website and the battle we pediatric nephrologists fight on this front.